

During anesthesia, arrhythmias can be produced in the presence of a variety of triggering agents and clinical situations such as light plane of anesthesia with hypertension and tachycardia, hypoxemia, and hypercarbia. Intracranial pathology such as subarachnoid hemorrhage and raised intracranial pressure can result in ECG abnormalities because of stimulation of the autonomic nervous system.Īirway manipulation most often associated with hemodynamic disturbances is a well-described cause of intraoperative arrhythmias. Patients with pre-existing heart disease (e.g., myocardial ischemia) have a much higher incidence of arrhythmias intraoperatively. Antiarrhythmic drugs act by modifying this action potential, which results from the alteration of ion channels ( Table 1). Each action potential corresponds to one beat of the heart and the inherent frequency of these cells is essential for maintaining proper rate control. In the heart, electrical stimulation is created by a sequence of ion fluxes through specialized channels in the cardiomyocytes that generate action potential and lead to a coordinated cardiac contraction in systole. The resting sinus heart rate in adults is usually between 60 and 100 beats/min.

From here, the impulse propagates to the atrioventricular node, then reaches the his bundle and Purkinje fibers transforming into conduction, causing ventricular contraction and generates the QRS wave.
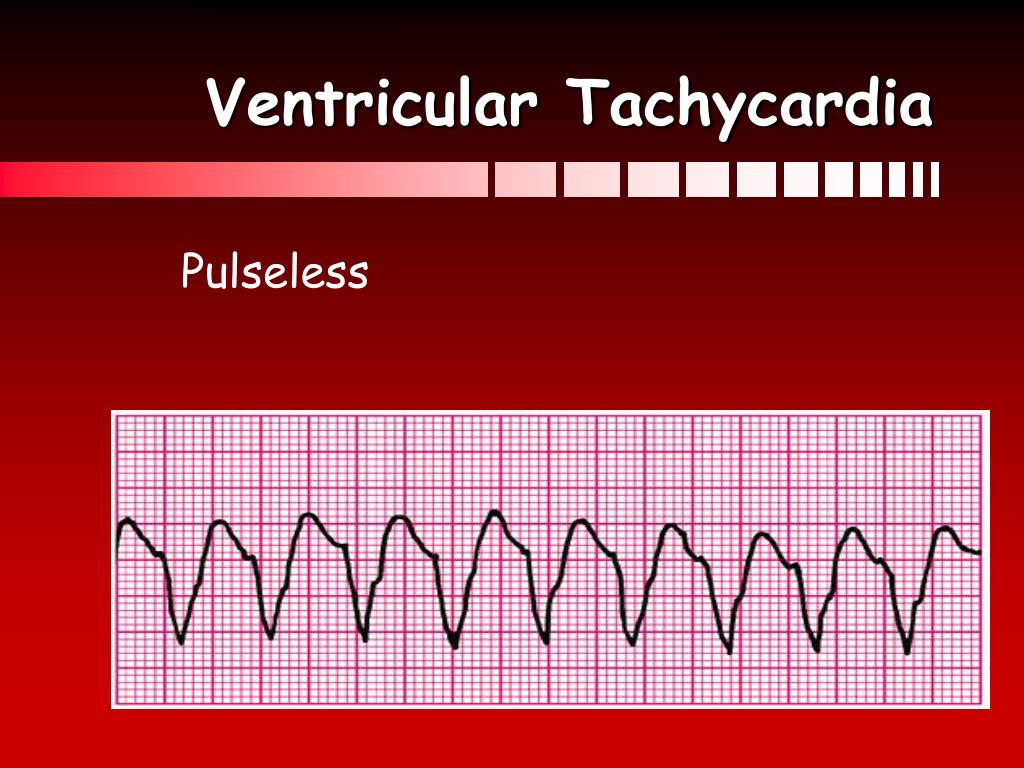
The atria depolarizes and generates the P wave. Normal cardiac conduction begins with cardiac impulses coming from the sinoatrial node and travels to both atria. The normal cardiac electrical conduction system is responsible for the contraction of the heart muscle and is represented on the electrocardiogram. Hence, a thorough understanding and prompt diagnosis and intervention are critical for the anesthesiologist in order to reduce severe perioperative adverse outcomes.Īn understanding of normal cardiac physiology is essential before rhythm disturbances can be understood. It is obvious that arrhythmias that occur during surgery are clinically important as it can evolve to life-threatening malignant arrhythmias with severe hemodynamic instability and cardiovascular collapse, necessitating prompt initiation of adequate cardiopulmonary resuscitation (CPR) and defibrillation or electrical cardioversion. Patients with pre-existing cardiac disease for cardiac surgery are more prone to develop perioperative rhythm disturbances. For cardiac surgery, the patients are more prone to develop arrhythmias with a reported incidence of greater than 90%, while incidence for patients undergoing non-cardiac surgery is lower and varies from 16.3 to 61.7%. While the incidence of perioperative arrhythmias is extremely high (the Multicenter Study of General Anesthesia reported a 70.2% incidence of Brady and tachyarrhythmias in 17,201 patients having general anesthesia for a variety of surgical procedures), only 1.6% of these required clinically significant management. Although ventricular tachycardia, ventricular fibrillation, torsade de pointes, and pulseless electrical activity are considered malignant arrhythmias that can lead to cardiac arrest, other types of Brady and tachyarrhythmias are also included in this chapter to enable adopting a more objective approach in the management of arrhythmias intraoperatively, avoiding risks of inappropriate management strategies.Īccelerated, slowed, or irregular heart rates caused by abnormalities in the electrical impulses of the myocardium.Ĭardiac arrhythmias are very common in the general population and are a significant cause of morbidity and mortality of both cardiac and noncardiac surgical procedures during the perioperative period. Treatment usually involves correction of the underlying causes, cardiac electroversion, and the use of one or more antiarrhythmic agents. Early diagnosis and commencement of an appropriate treatment protocol may be lifesaving.
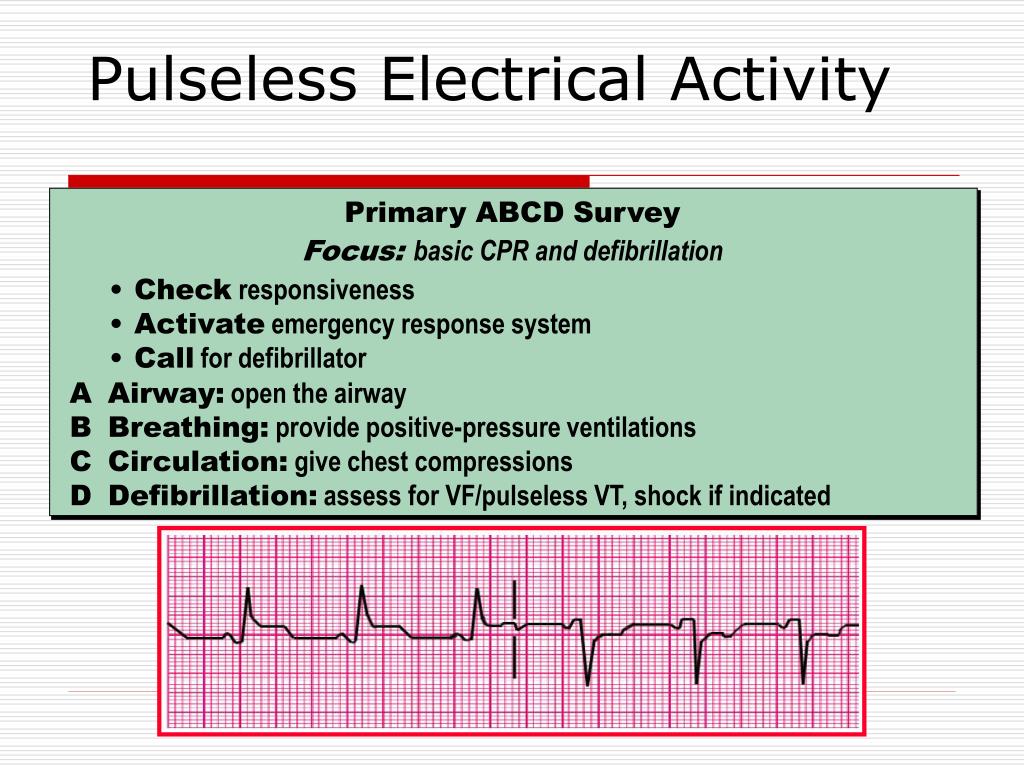
Predisposing factors like electrolytes abnormalities, pre-existing cardiac disease, intubation procedure, anesthetic medications, and various surgical stimulation need to be determined. They result in a significant cause of morbidity and mortality, particularly in elderly patients. Life-threatening arrhythmias are frequently encountered during anesthesia for cardiac or non-cardiac surgery.


 0 kommentar(er)
0 kommentar(er)
